
Led by Associate Professor Charlotte Albury at the University of Oxford, this CPD-certified project aims to develop a supportive and motivational online learning tool that provides primary care professionals with practical conversational techniques grounded in real-world evidence.
Research shows that primary care practitioners often face challenges when discussing weight loss with patients, whether it’s starting the conversation or managing resistance. This project offers a simple approach to addressing these challenges through a co-designed, evidence-based learning tool that practitioners can easily integrate into their work.
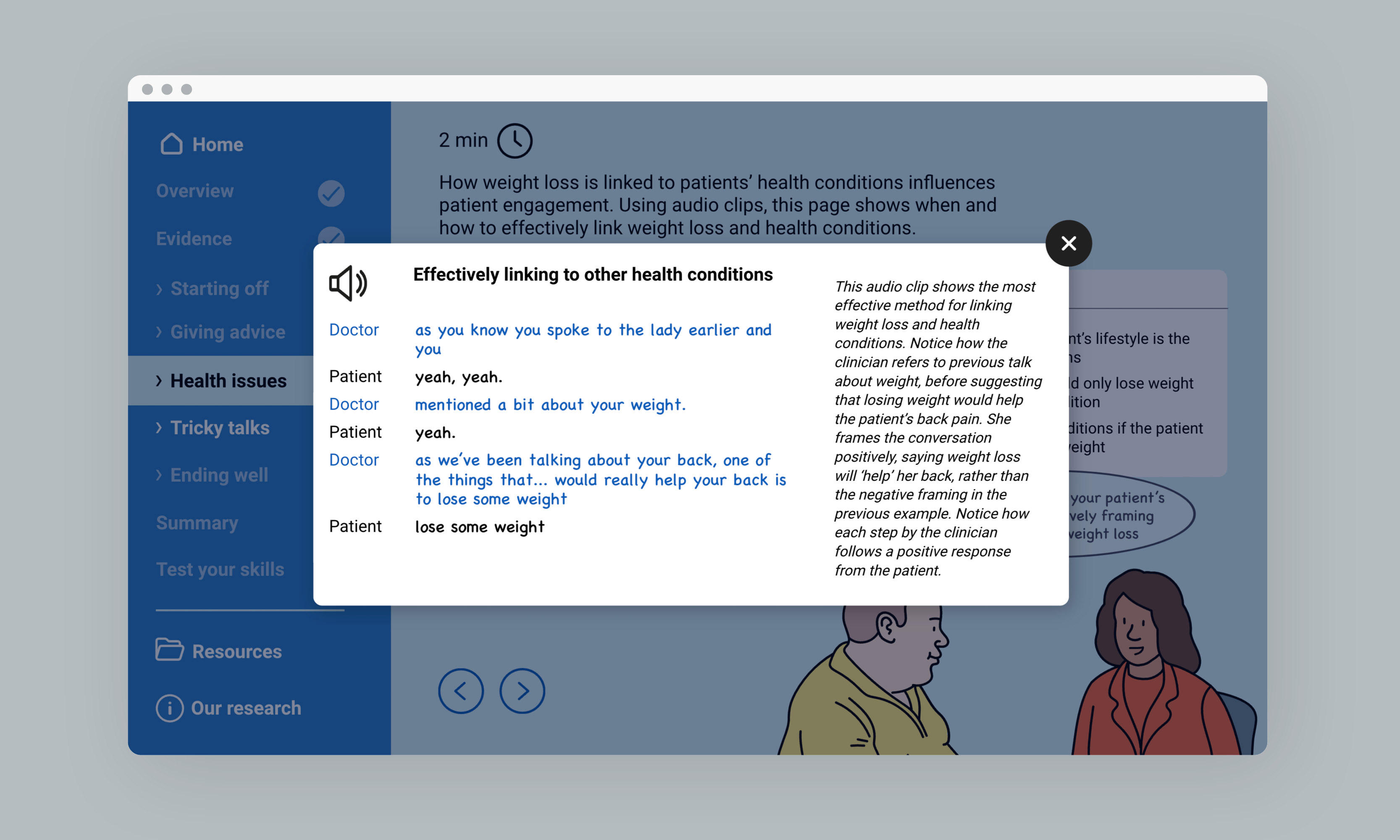
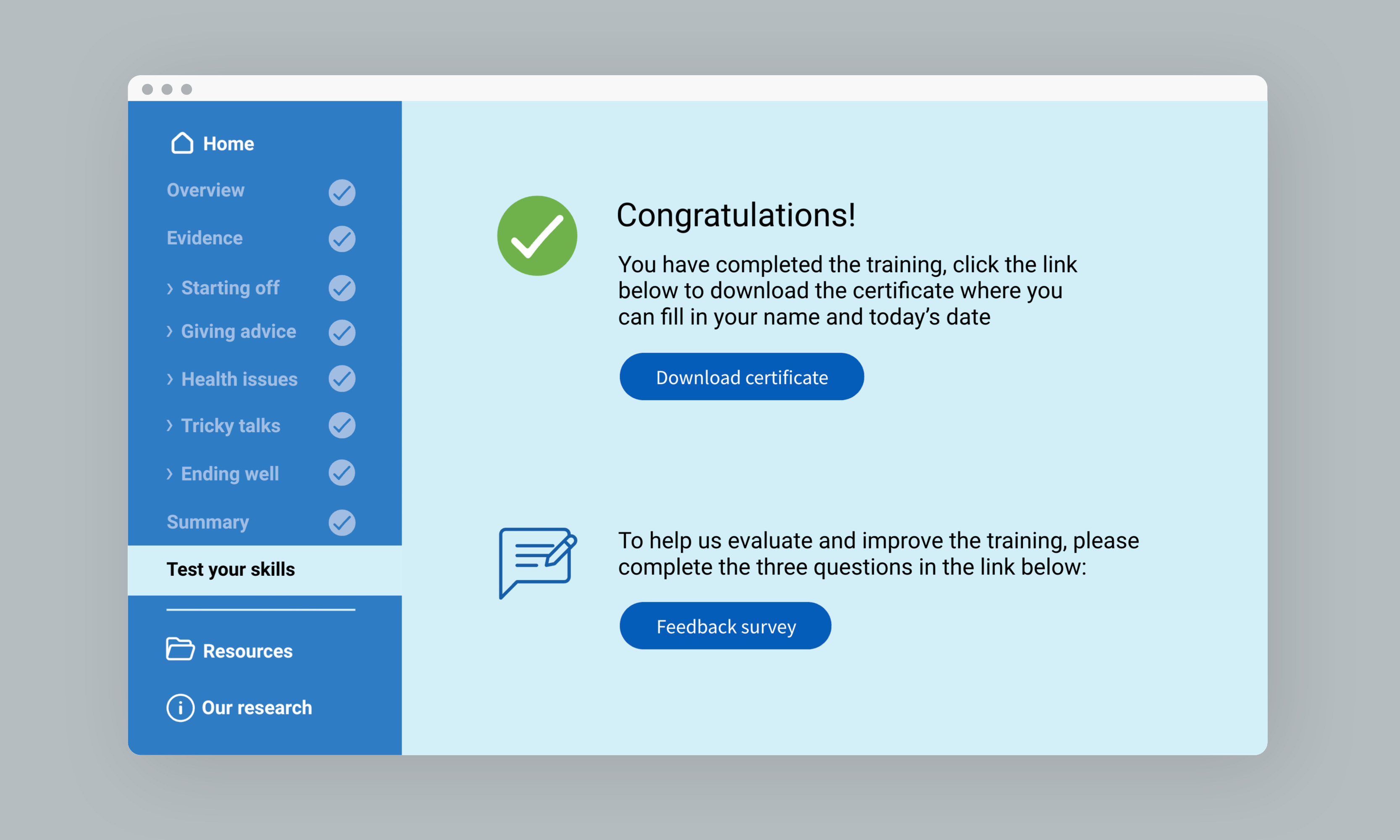
Our online learning tool is designed to help practitioners navigate delicate conversations about weight management by providing strategies for incorporating brief, effective discussions into consultations. The tool is based on real interactions between healthcare providers and patients, offering practical tips for navigating difficult moments with empathy and care.
Key elements include:
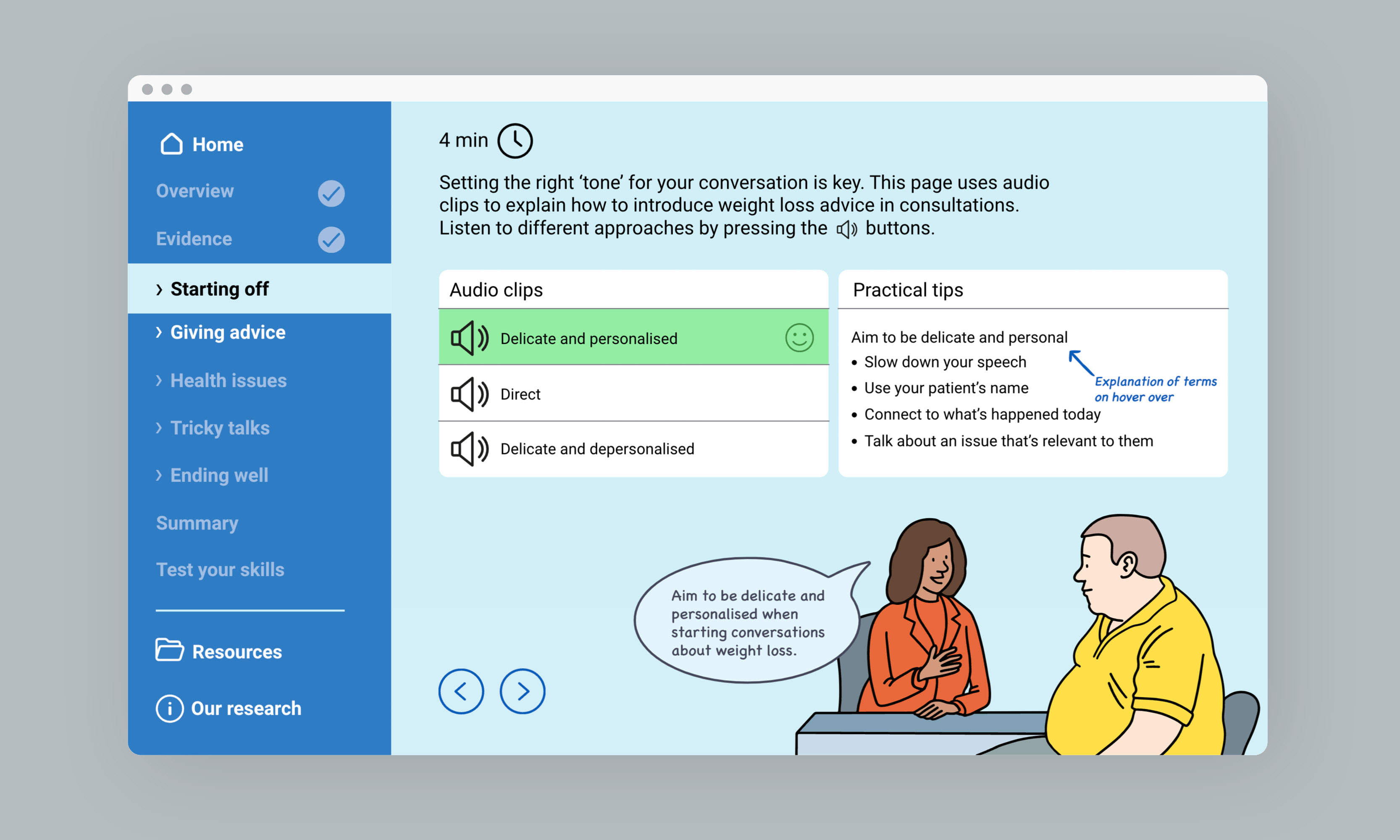
Practitioners often feel underprepared to discuss weight management, with limited time and training as significant barriers. Our learning tool focuses on quick, impactful conversations that can fit into their appointments. This approach is vital, as conversations about weight are sensitive and must be handled with care, avoiding directness that could lead to resistance.
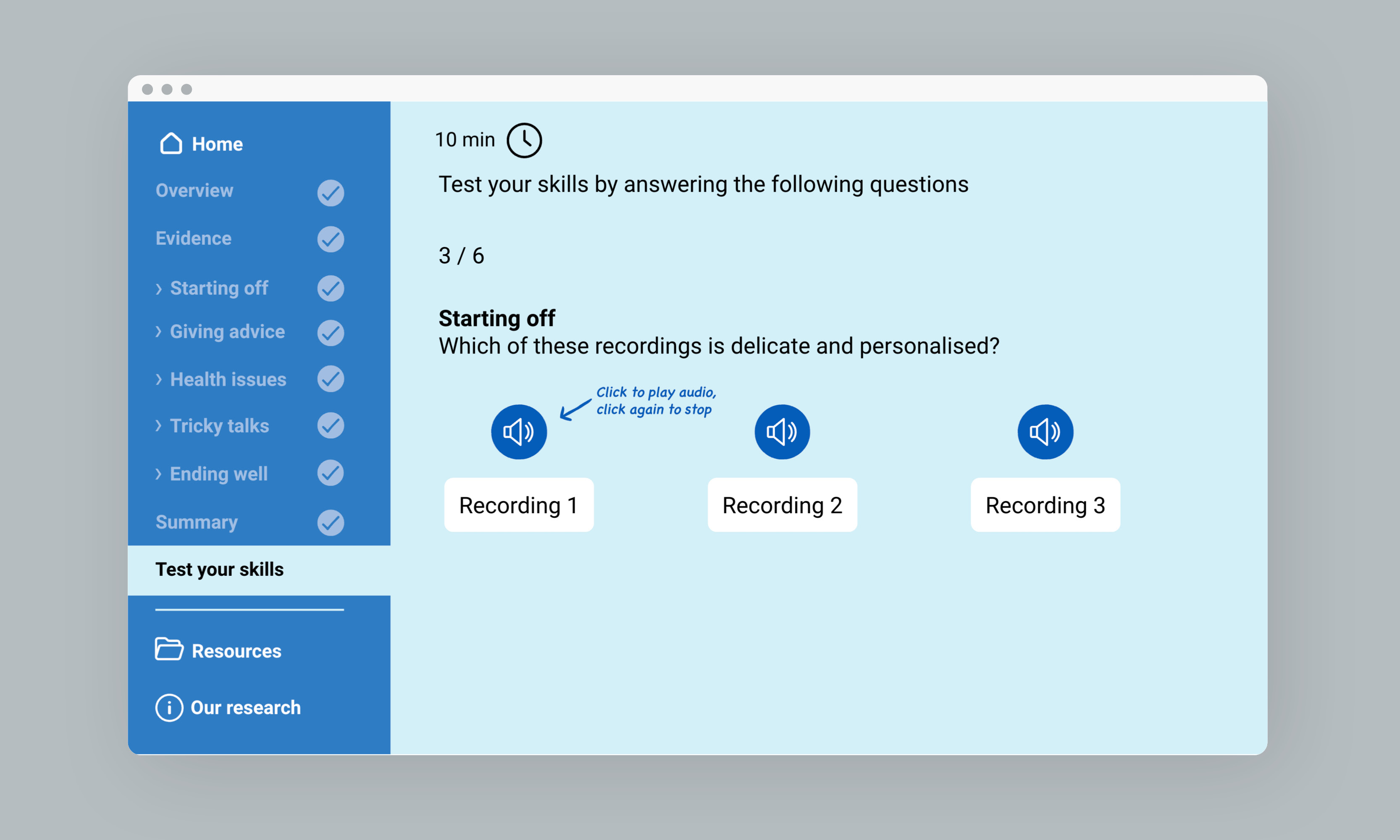
The learning module addresses this through its seven trainable areas:
Our approach ensures that practitioners can practise and refine these strategies, making every patient conversation a potential catalyst for positive change.
Throughout the project, we held workshops with both practitioners and patients, refining the design to ensure it meets their needs. In these workshops, we tested everything from tone of voice to visual design, ensuring the tool is both practical and engaging.
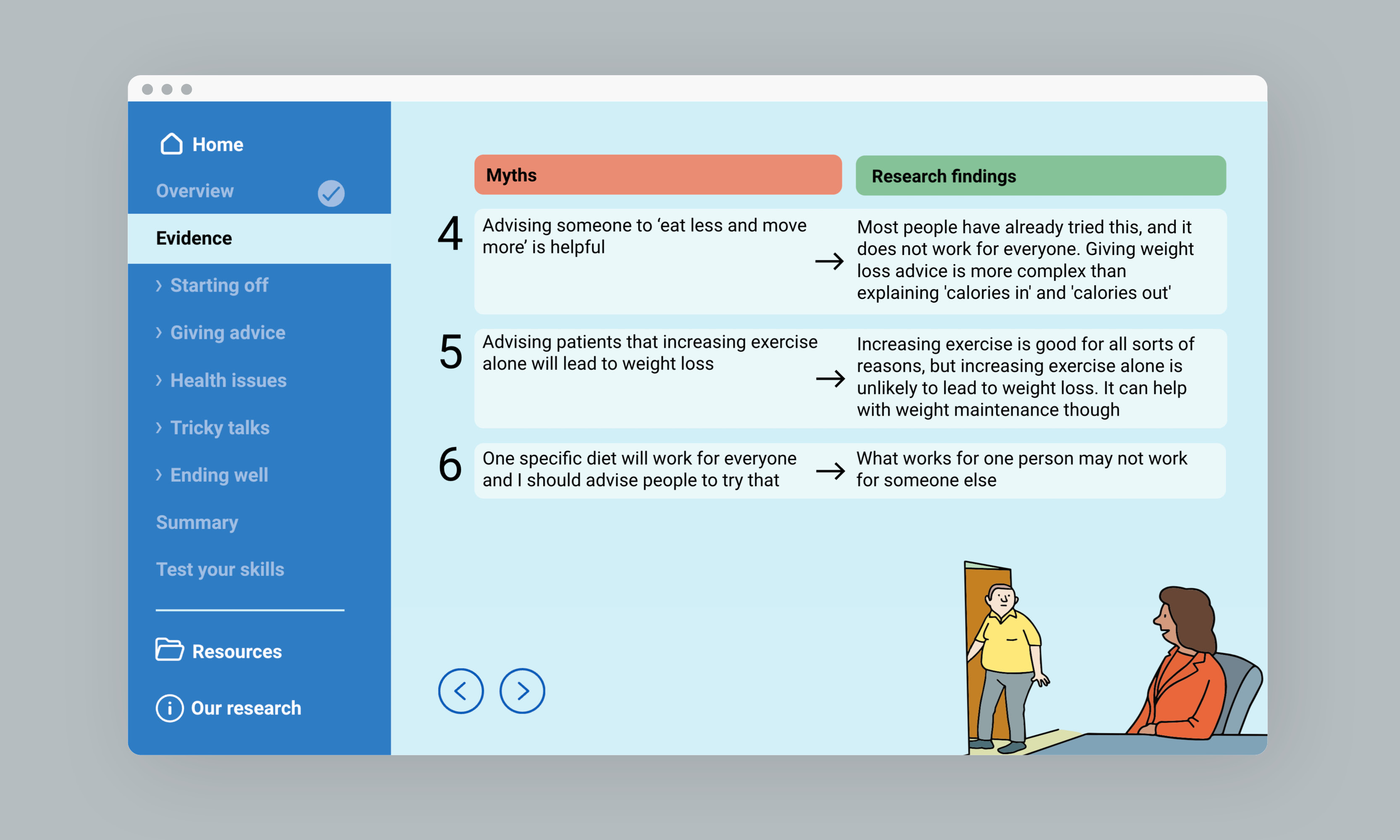
For example, during a practitioner workshop, we heard about the challenges that GPs have in starting conversations as well as suggestions on where to publicise the training module when ready. We also heard that some of the myths associated with weight loss were still in common practice, for example using health coaching and motivational interviewing or thinking that you could only mention weight loss during a consultation dedicated to the subject.
Similarly, patient workshops provided insight into how patients perceive conversations about their weight. We learned that patients prefer discussions that are non-judgemental and that avoid patronising comments like, ‘you must do this‘ Patients felt that practitioners should avoid imposing their own attitudes and assumptions, such as assuming patients are ‘struggling‘ with weight issues. They wanted conversations to be personalised taking into account things like bereavement, poverty, cultural backgrounds, family dynamics and health conditions. Ultimately, they wanted practitioners to develop empathy and soft skills, to recognise the emotional and psychological factors tied to weight gain, to get better training around empathy and to avoid making patients feel like they were being ‘talked at‘, creating an ‘us versus them‘ dynamic.
We are preparing for the module’s launch with a social media campaign aimed at raising awareness across healthcare networks and promoting the learning tool as it is rolled out to practitioners.
By offering practical, evidence-based tools, we aim to empower primary care practitioners to have short and motivational conversations with their patients about weight loss, ultimately improving patient outcomes.
If you’re passionate about enhancing healthcare impact through design, we’d love to hear from you.